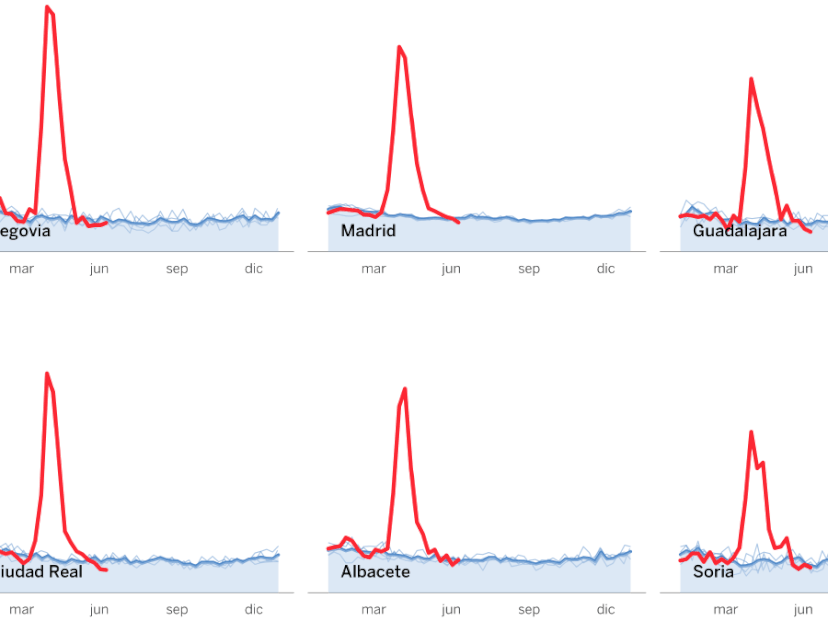
An analysis of three Covid-19 outbreaks: how they happened and how they can be avoided
An office, a restaurant and a bus were the settings for multiple infections that have been studied in detail by health authorities. Their conclusions offer valuable lessons for the deescalation process
A crowded restaurant to celebrate the Chinese New Year; 100 workers infected inside a 19-story building; a group of devout Buddhists travelling by bus for a religious ceremony. These were the scenarios for three outbreaks of Covid-19 that have been carefully documented by the authorities. What happened in each one? What were the risk factors? What lessons can be learned, now that we are trying to get back to normal and return to restaurants, offices and other shared spaces?
The office
In a single wing of a call center in Seoul, in South Korea, the risk of infection was multiplied by four key factors: close, prolonged contact between numerous people, in an enclosed space.
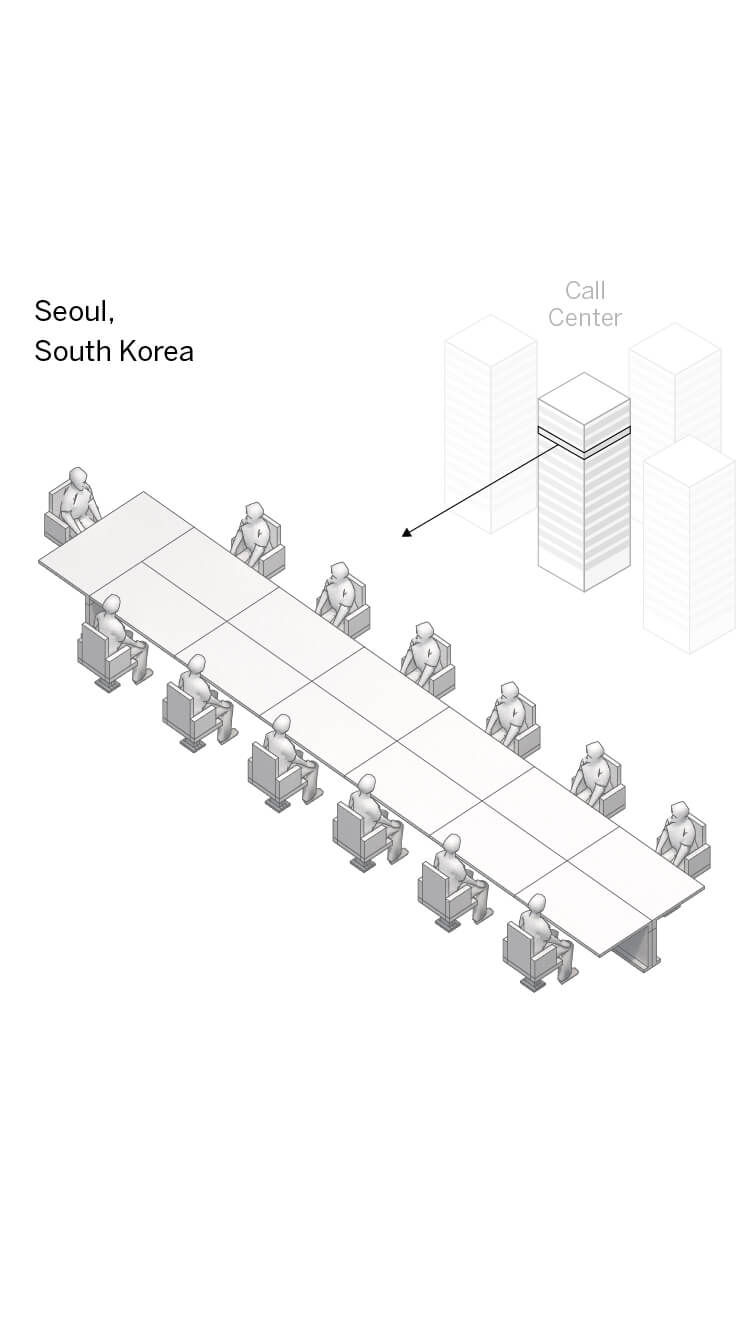
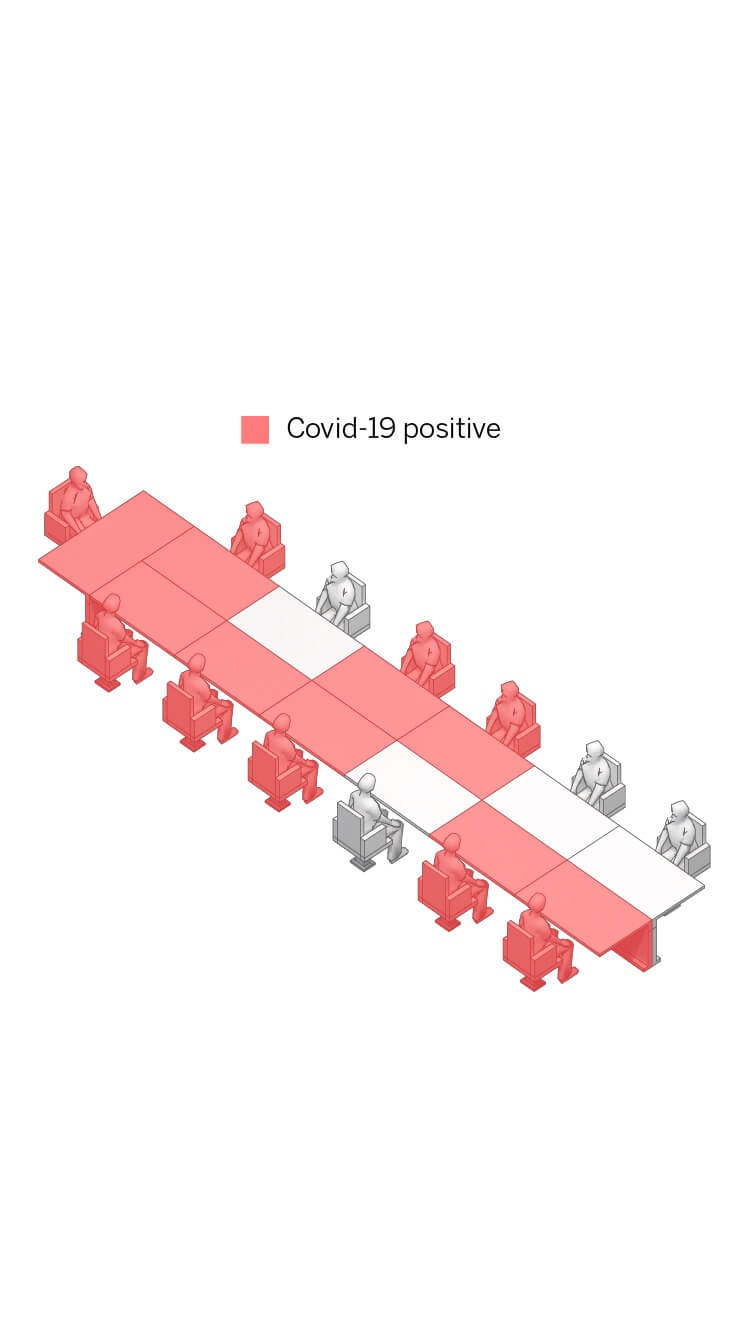
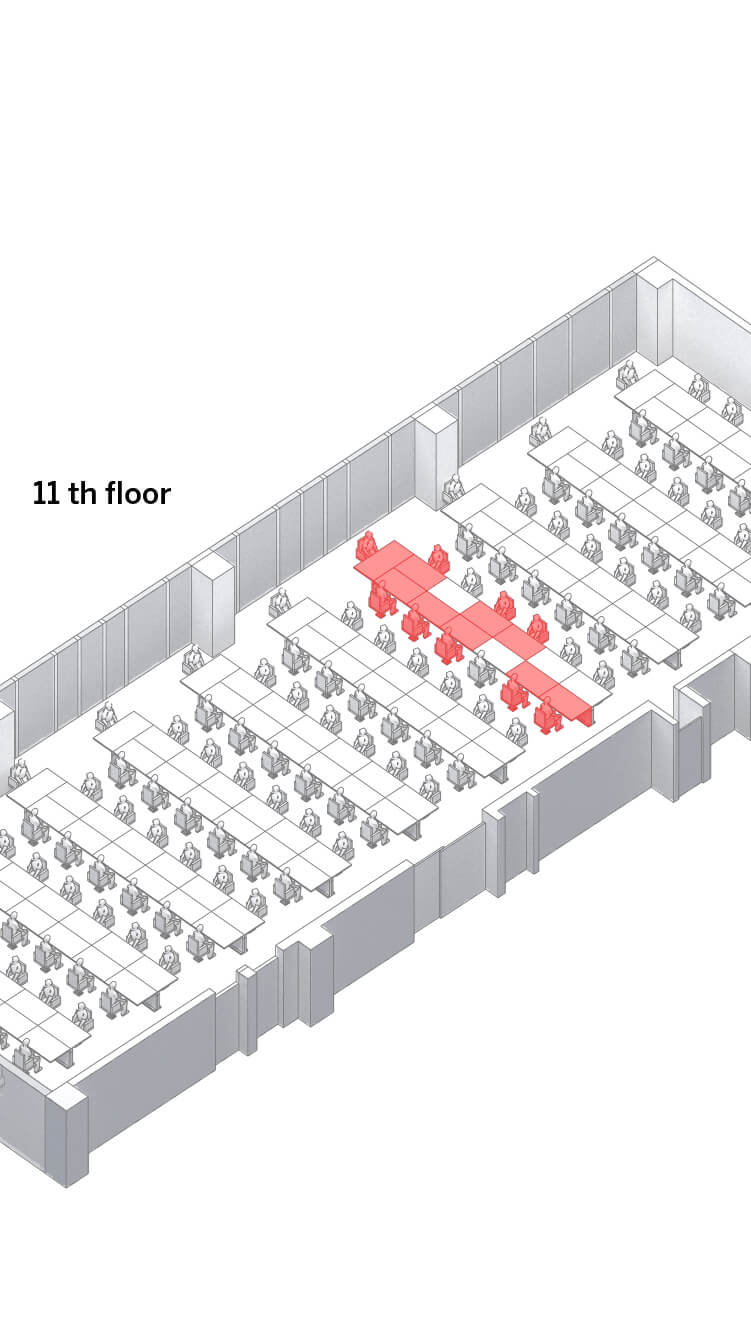
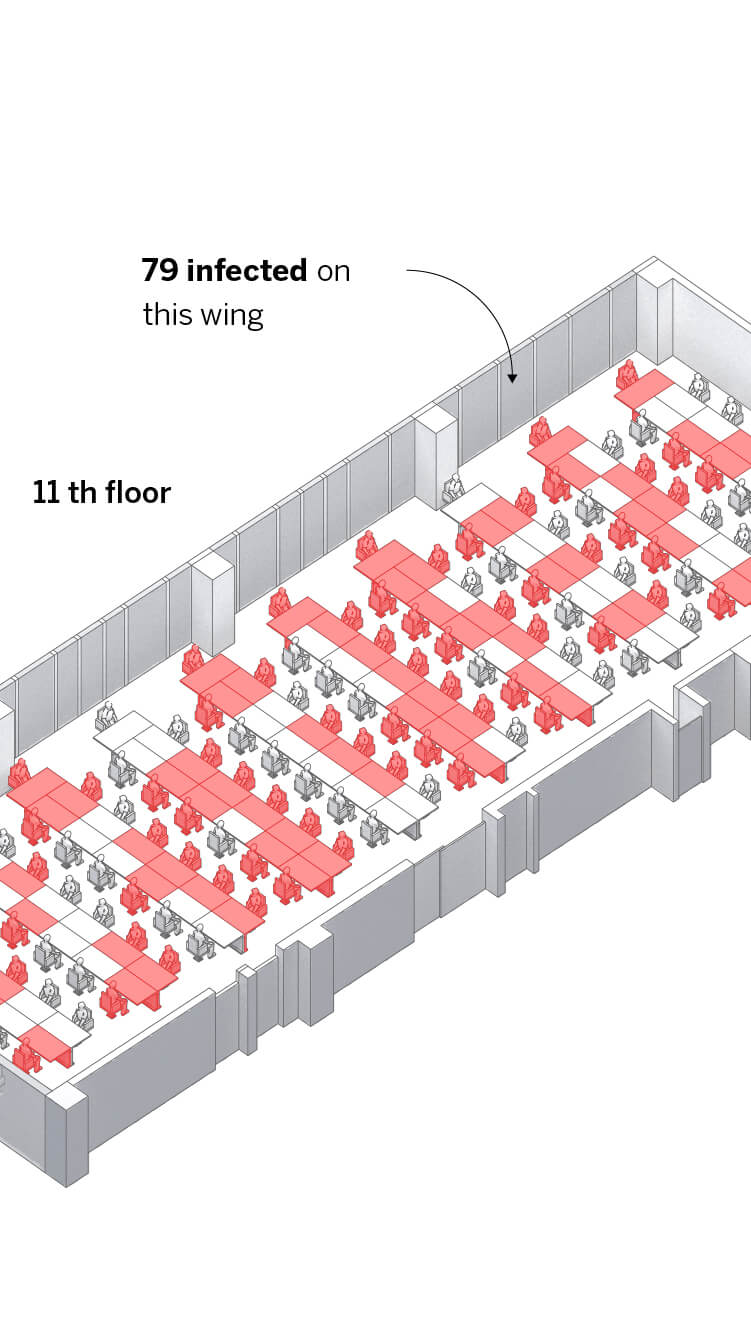
The staff at the call center on the 11th floor work together at desks containing 13 work stations.
On some desks, such as this one, nine of the 13 employees tested positive.
These employees were sitting inside an enclosed space with 137 workers.
Out of these 137 employees, 79 (57.6%) tested positive. The permanent contact within the same space over a prolonged period of time played a crucial role.
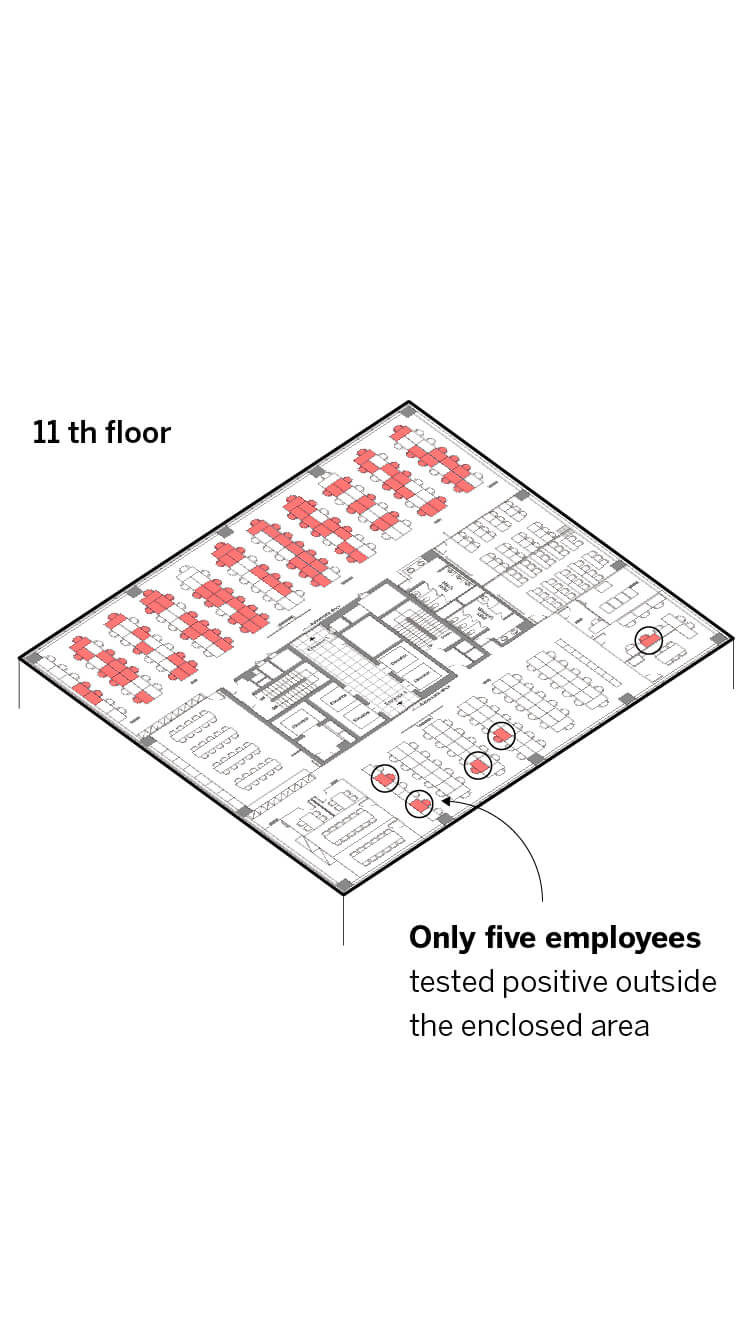
Far fewer of the other employees on this floor tested positive.
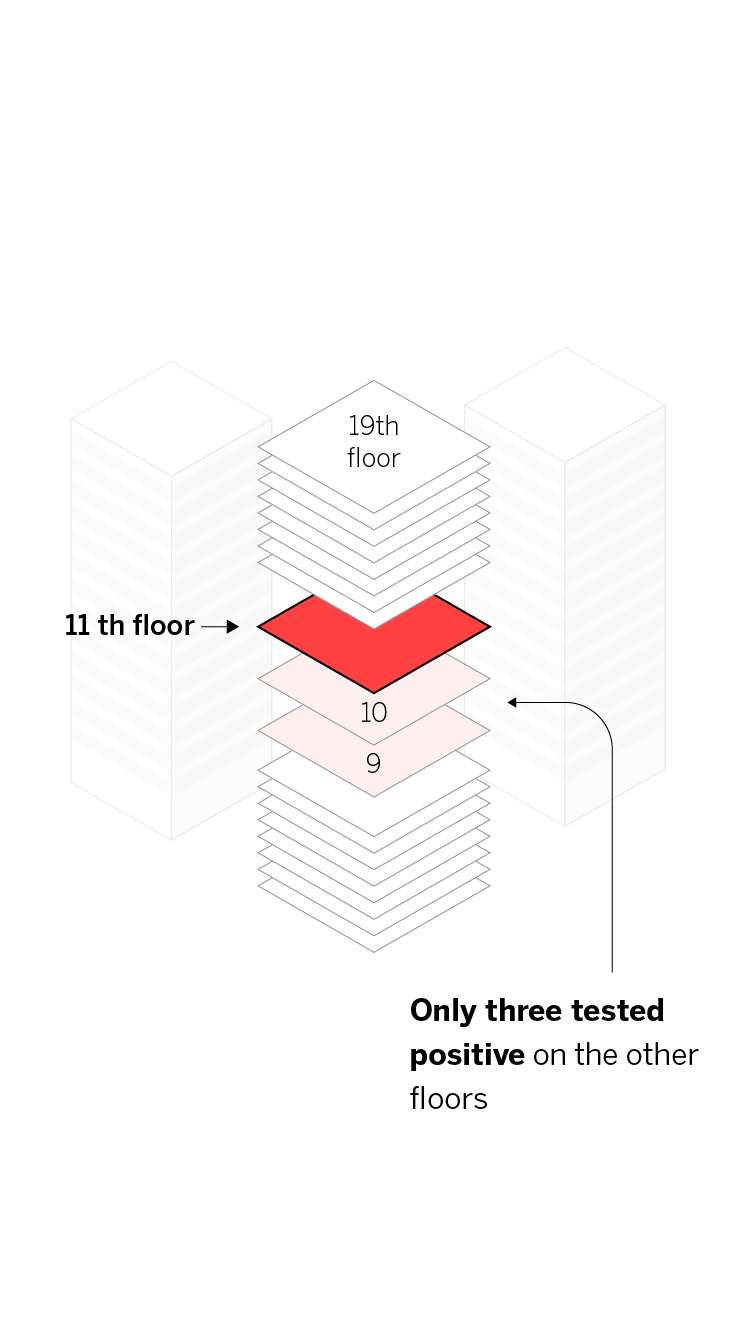
In the rest of the building, only three people tested positive out of 927 who underwent checks (0.3%) despite the fact they shared lobbies, elevators and other communal areas.
Research carried out by local authorities revealed that almost all the people infected in a 19-story building with more than a thousand residents and office workers were confined to this area. Moreover, those infected were almost exclusively working in the same room. Despite the considerable interaction between workers from different floors of the building in the elevators and the lobby, the spread of the virus was largely confined to that one space filled with employees sitting at desks, “indicating that the duration of the interaction (or contact) was probably the main facilitator for extensive infection,” according to the Seoul authorities’ report.
Recommendations from scientists and health experts aim to diminish the risk by avoiding large concentrations of people with measures ranging from taking turns to remote work to using physical protection such as masks and preventing employees from sharing office materials. The recommendations also include physically distancing staff by cutting out big meetings and keeping numbers low at access points and in food and drink zones; spaces should also be properly ventilated. “We must reduce the concentration of people and exposure time, the time they spend together,” says Maricruz Minguillón, a researcher at the Spanish National Research Council’s Institute of Environmental Assessment and Water Studies (IDAEA-CSIC). “If we reduce both factors, we reduce the risk.”
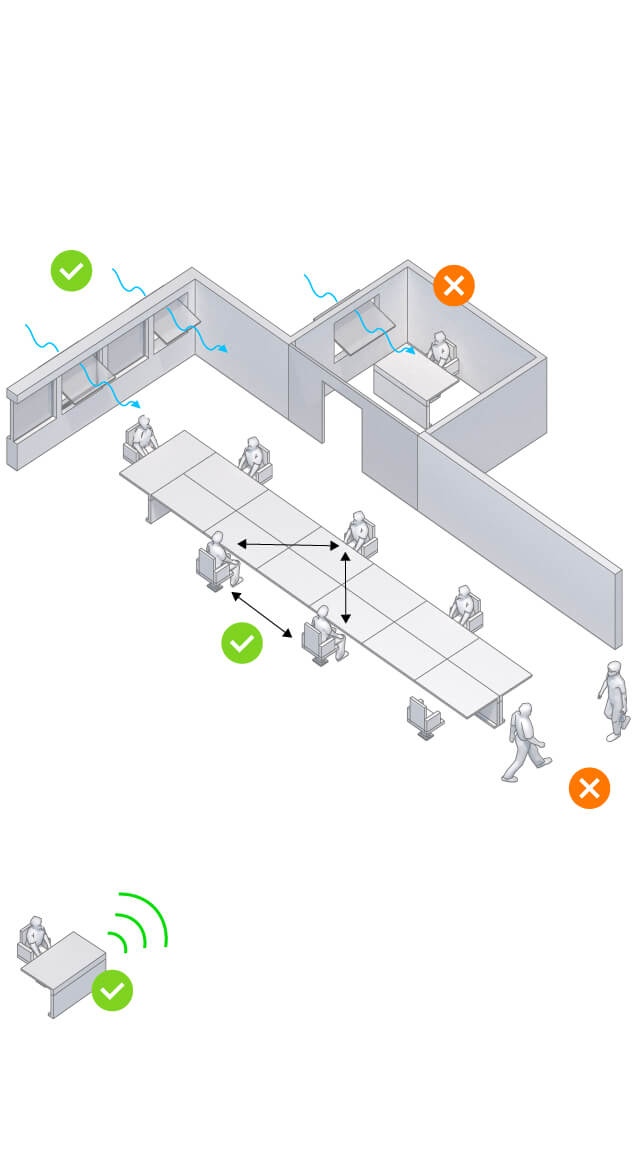
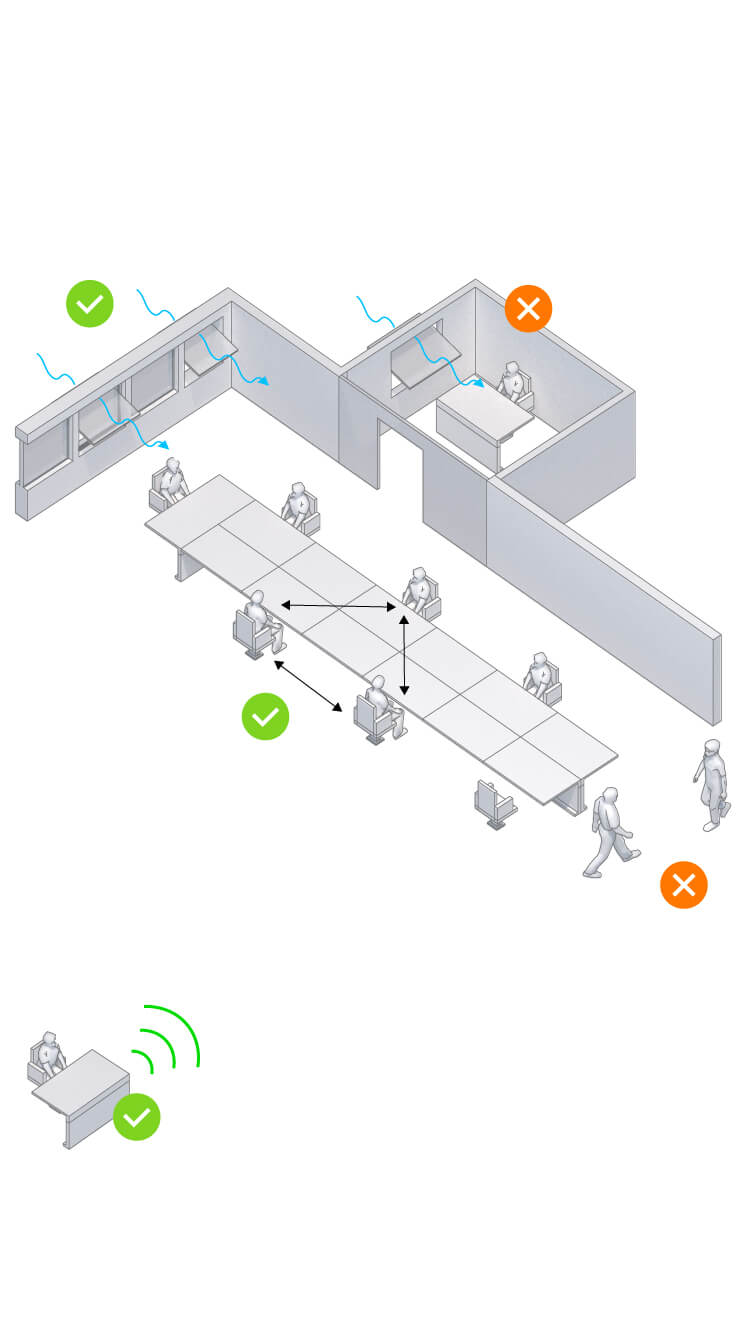
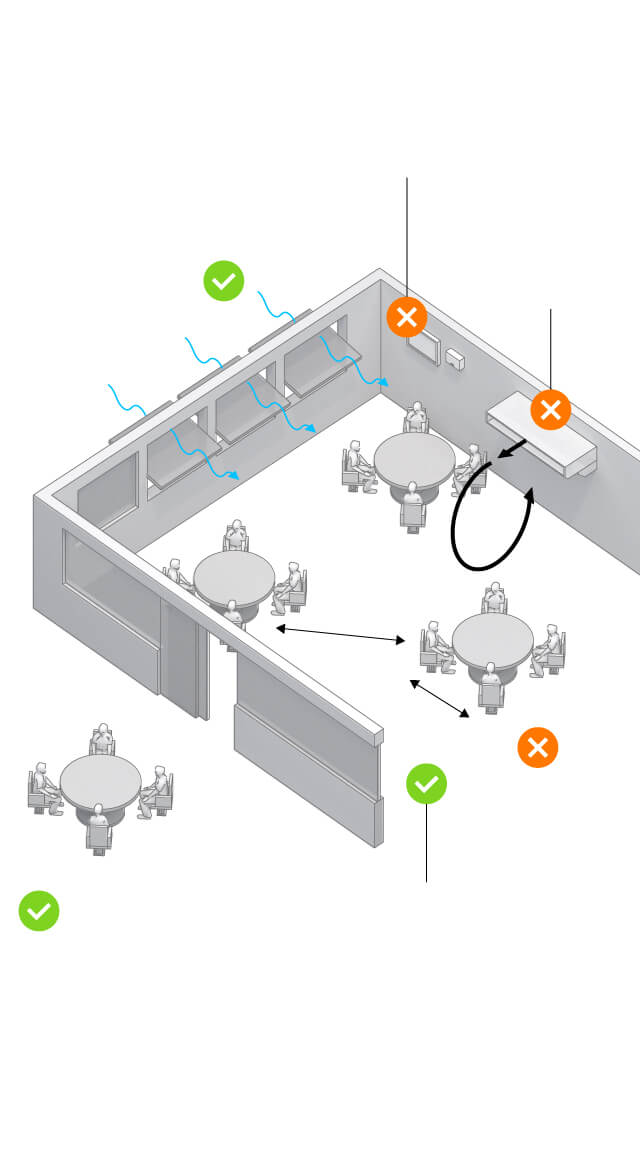
How it can be avoided
Natural ventilation to avoid the recirculation of infected particles
Avoid concentrations of employees either in meetings or in food and drink zones
2 m.
Organize workstations in a zig-zag pattern and maintain a distance of two meters between each
Avoid physical contact.
No sharing of material or equipment between co-workers without prior disinfection
Keep staff distanced by combining teleworking with flexitime
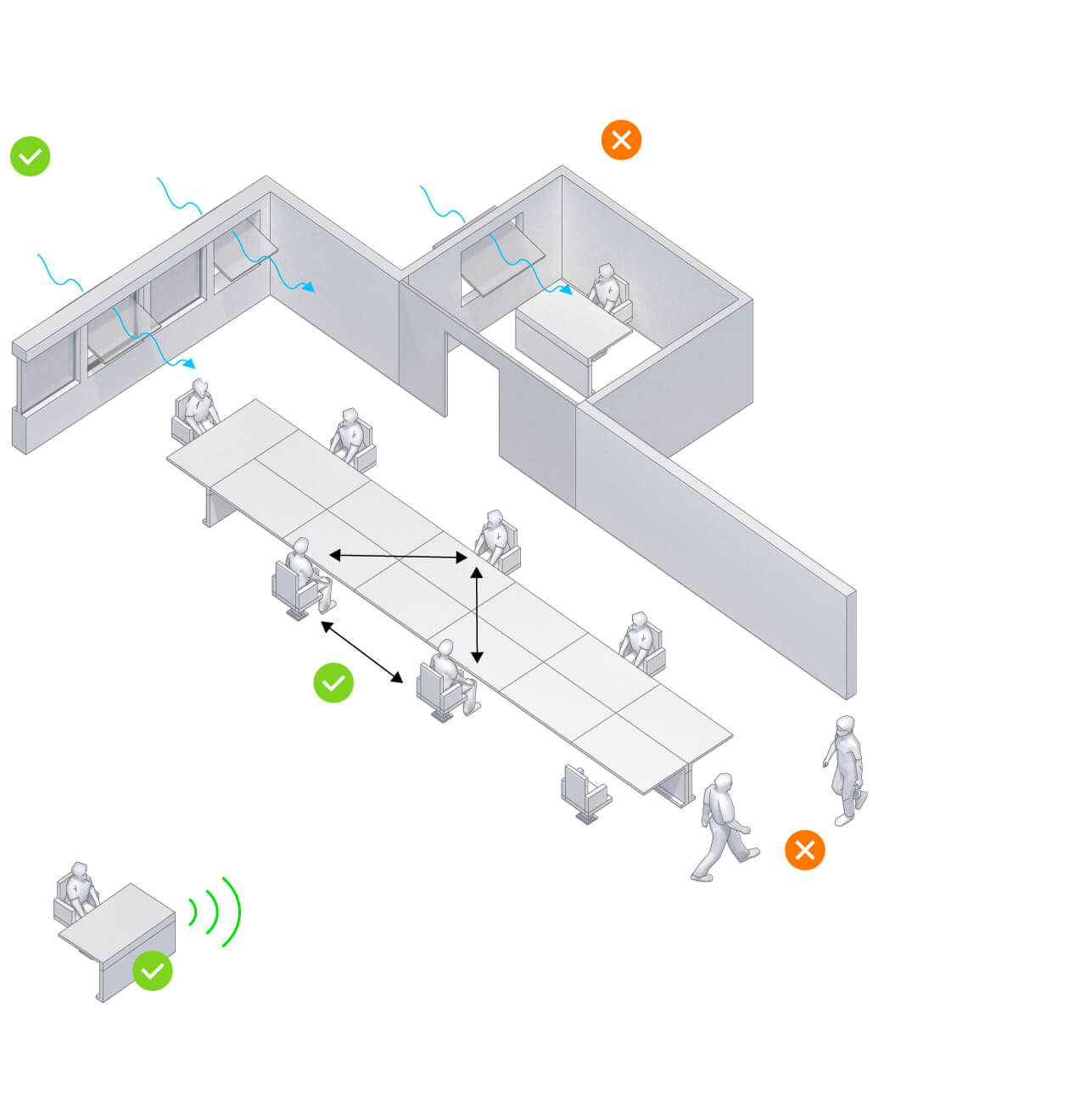
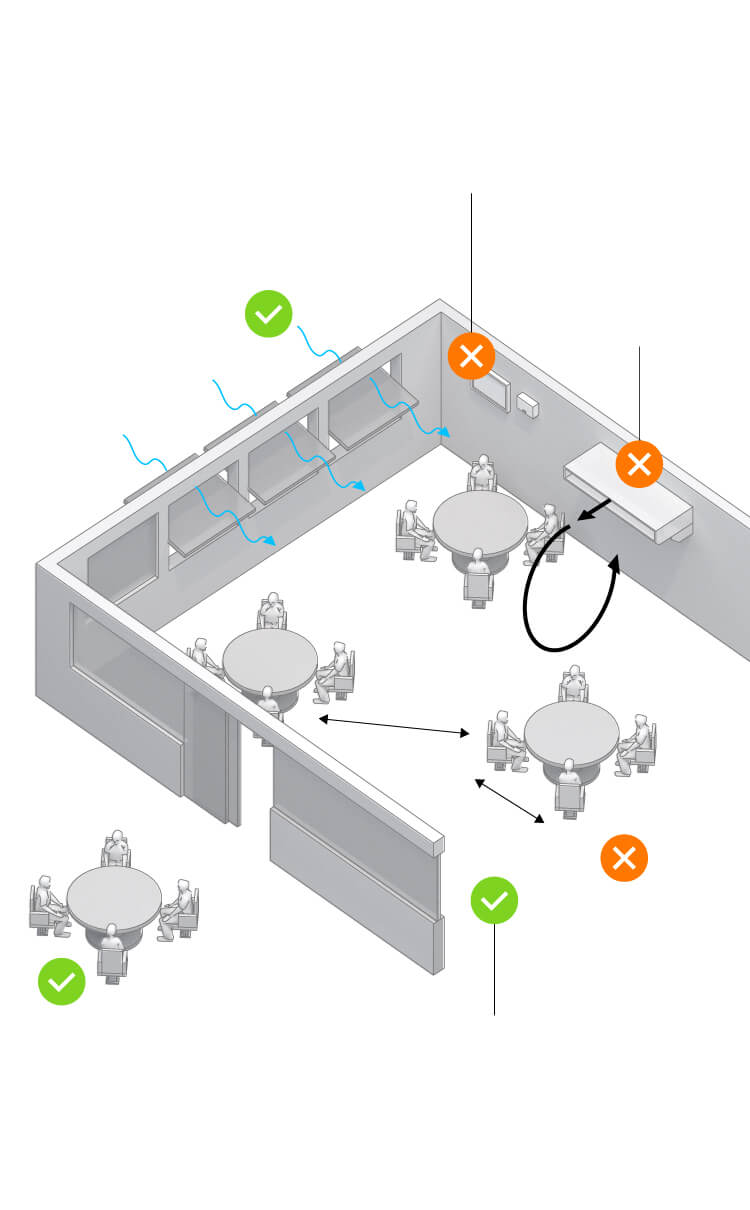
How it can be avoided
Avoid concentrations of employees either in meetings or in food and drink zones
Natural ventilation to avoid the recirculation of infected particles
2 m
Organize workstations in a zig-zag pattern and maintain a distance of two meters between each
Avoid physical contact.
No sharing of material or equipment between co-workers without prior disinfection
Keep staff distanced by combining teleworking with flexitime
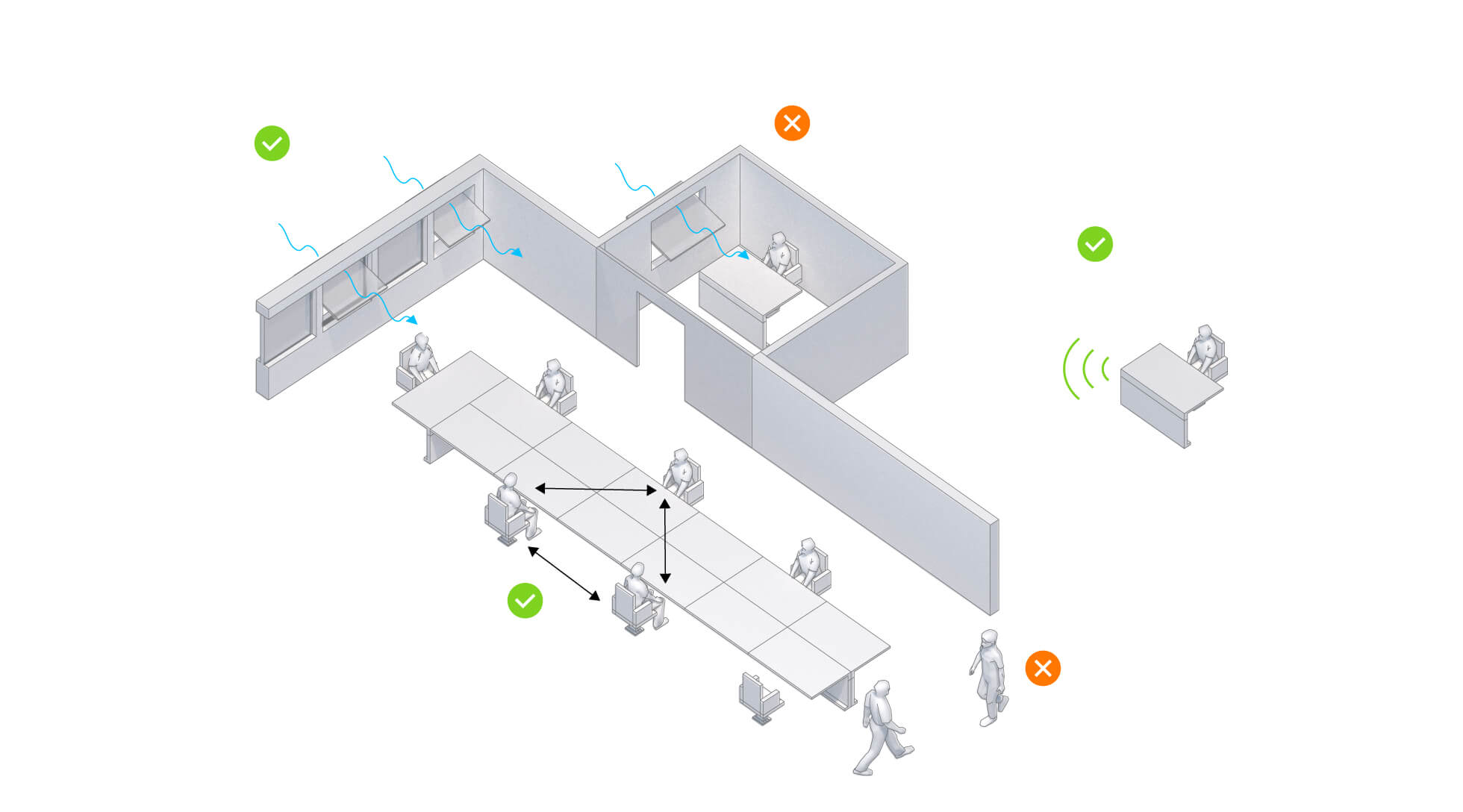
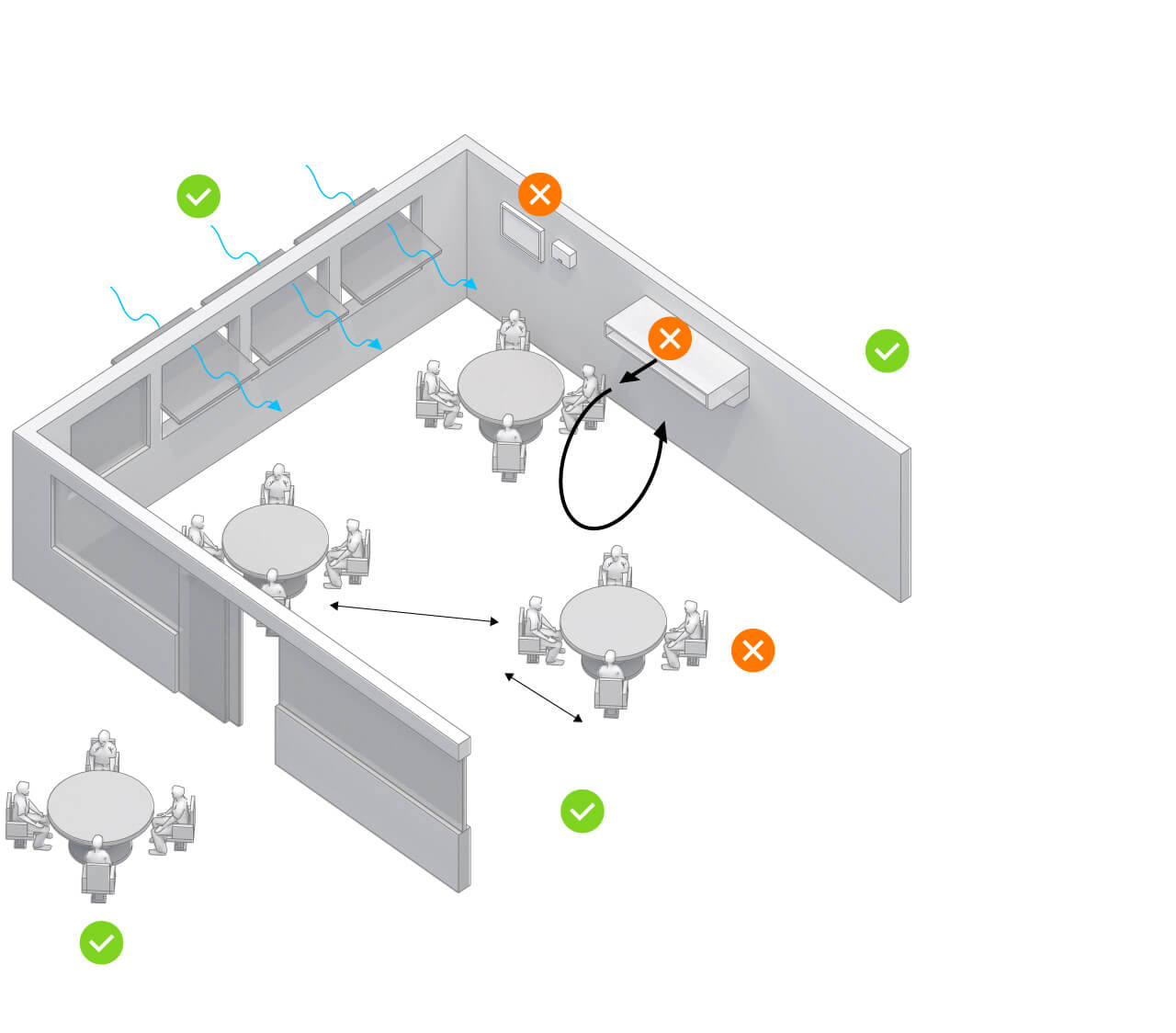
How it can be avoided
Natural ventilation to avoid the recirculation of infected particles
Avoid concentrations of employees either in meetings or in food and drink zones
2 m
Organize workstations in a zig-zag pattern and maintain a distance of two meters between each
Avoid physical contact.
No sharing of material or equipment between co-workers without prior disinfection
Keep staff distanced by combining teleworking with flexitime
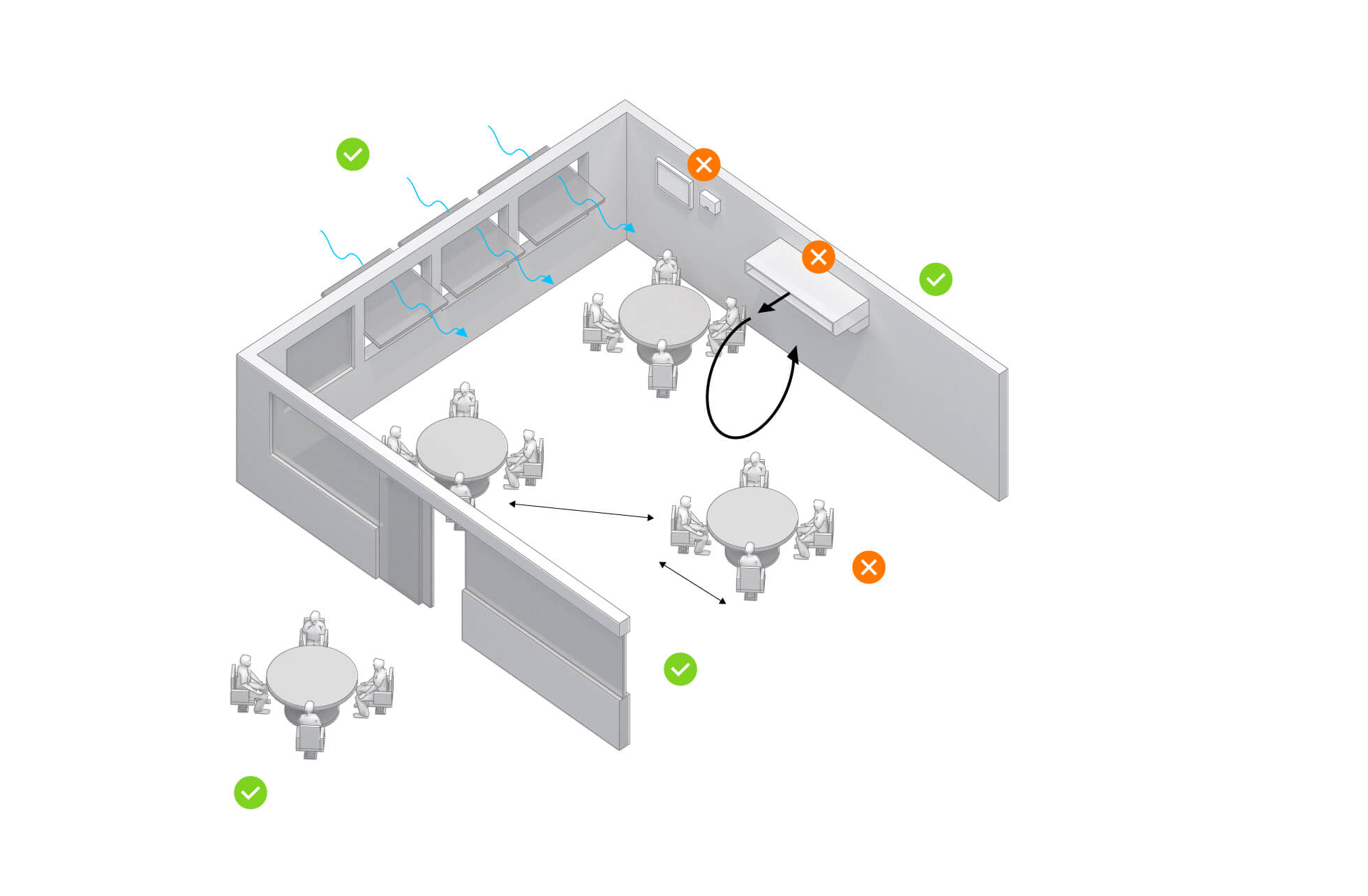
How it can be avoided
Natural ventilation to avoid the recirculation of infected particles
Avoid concentrations of employees either in meetings or in food and drink zones
Keep staff distanced by combining teleworking with flexitime
2 m
Organize workstations in a zig-zag pattern and maintain a distance of two meters between each
Avoid physical contact.
No sharing of material or equipment between co-workers without prior disinfection
The restaurant
A New Year’s meal in the Chinese city of Guangzhou on January 24 provides the best example of how to reduce indoor risks. This scenario has been analyzed in detail in two different studies (1, 2) by the Chinese health authorities, who concluded that poor ventilation can be a decisive risk factor if contact is maintained during prolonged periods. Again, time plus social proximity multiplies the risks.
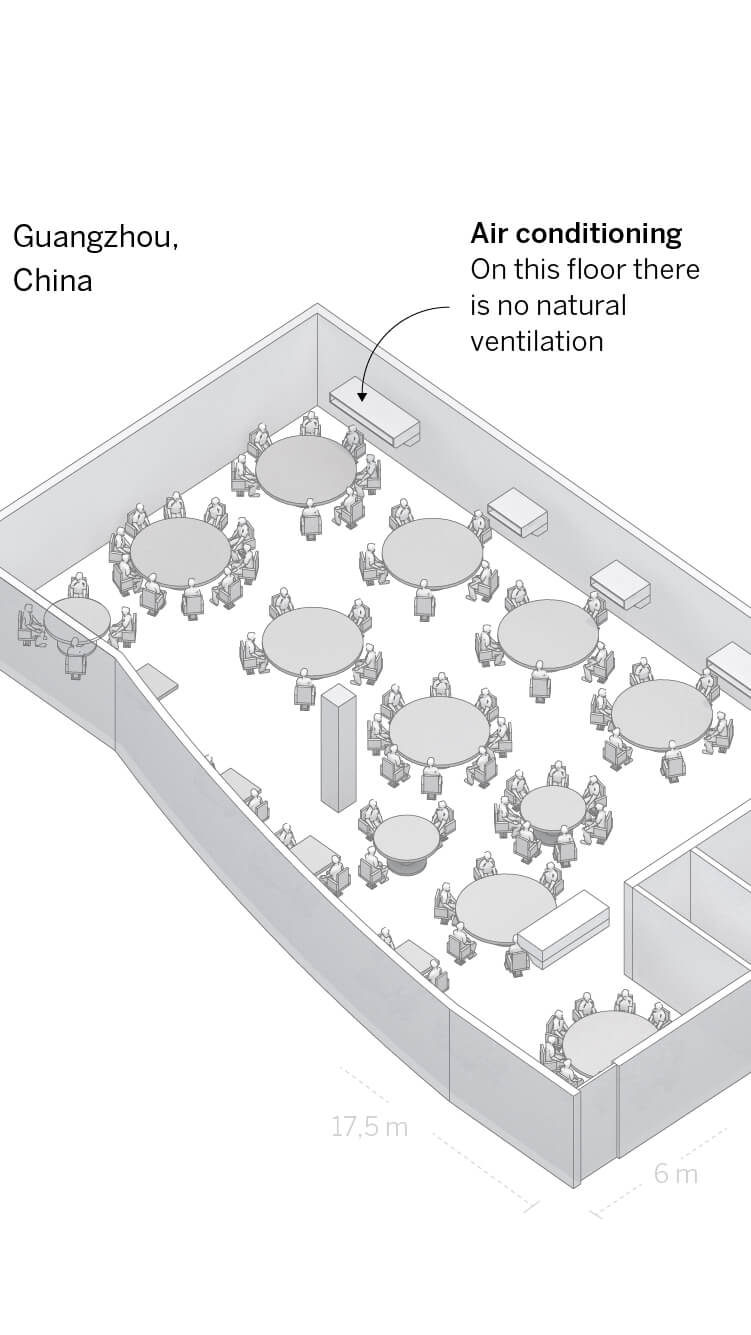
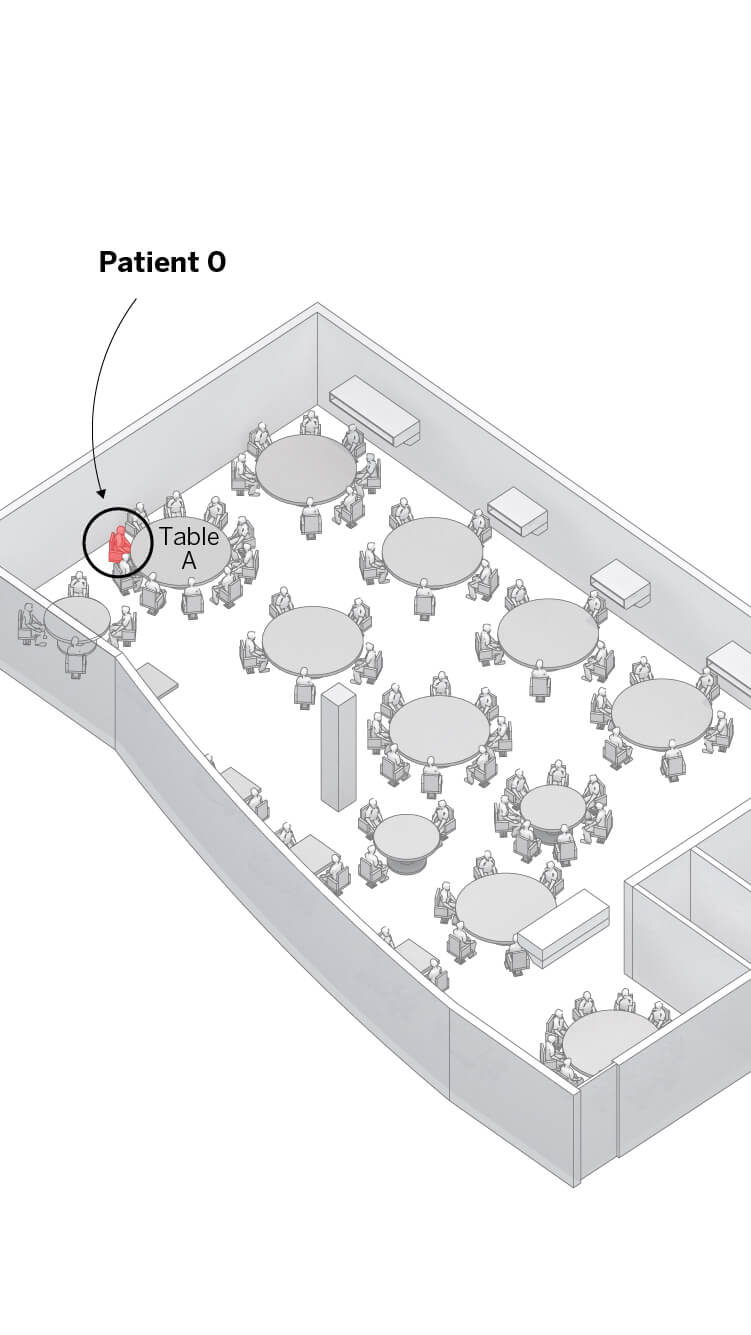
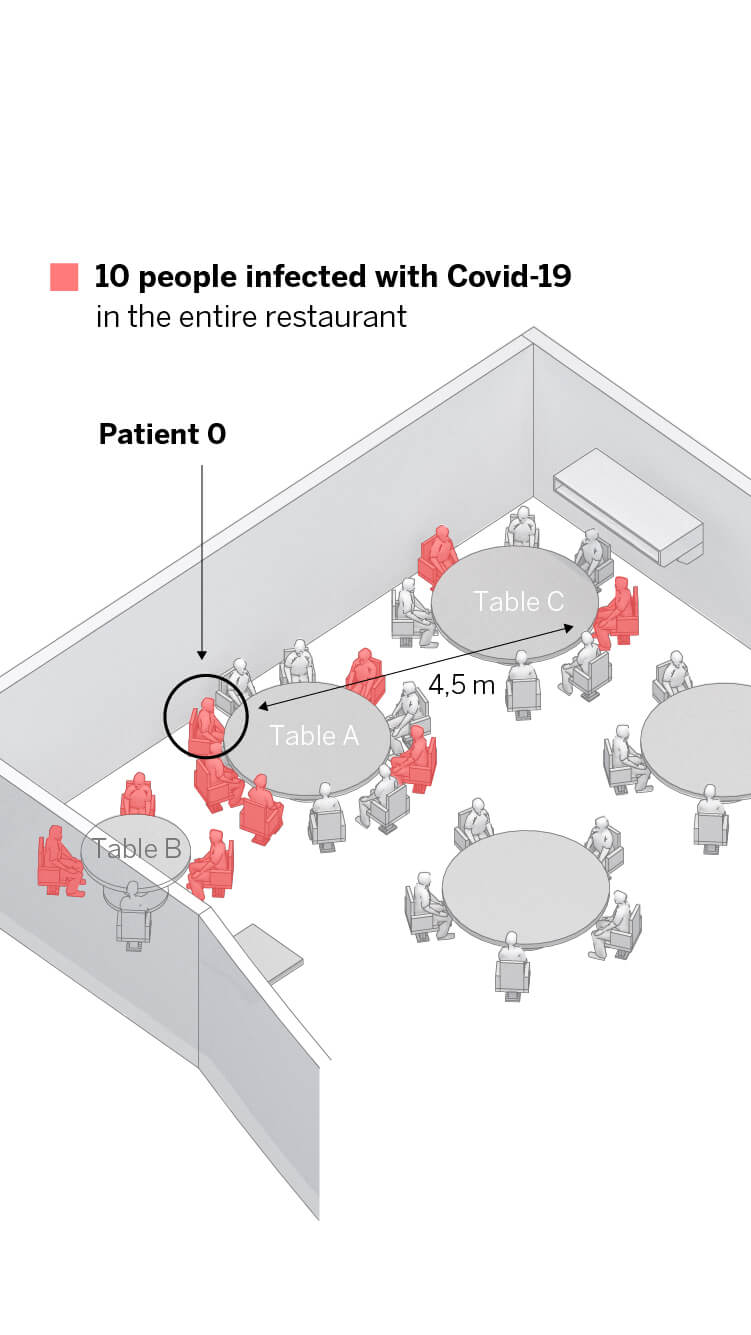
The restaurant was full the day of the celebrations. The outbreak happened in a room with no natural ventilation where around 90 people were eating with eight waiters serving.
On table A, a person who had arrived the day before from Wuhan was eating with their family. That night, that person showed symptoms and went to hospital.
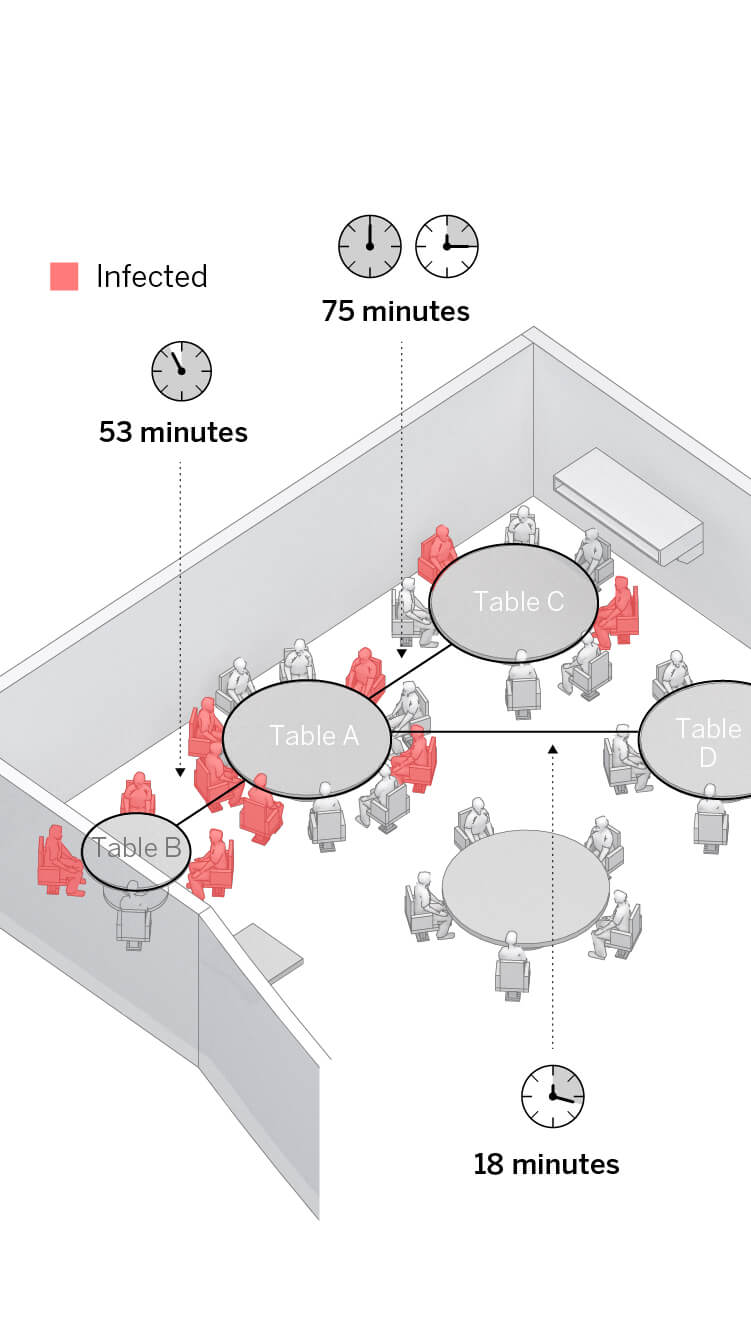
After the meal, another nine customers were diagnosed with Covid-19. All those infected from tables B and C were more than a meter away from Patient 0, some as far as 4.5 meters. No one else in the restaurant became infected.
Length of time is critical. The meals of families B and C overlapped with that of Patient 0 for an extended period, while those at table D only overlapped with Patient 0 for 18 minutes.
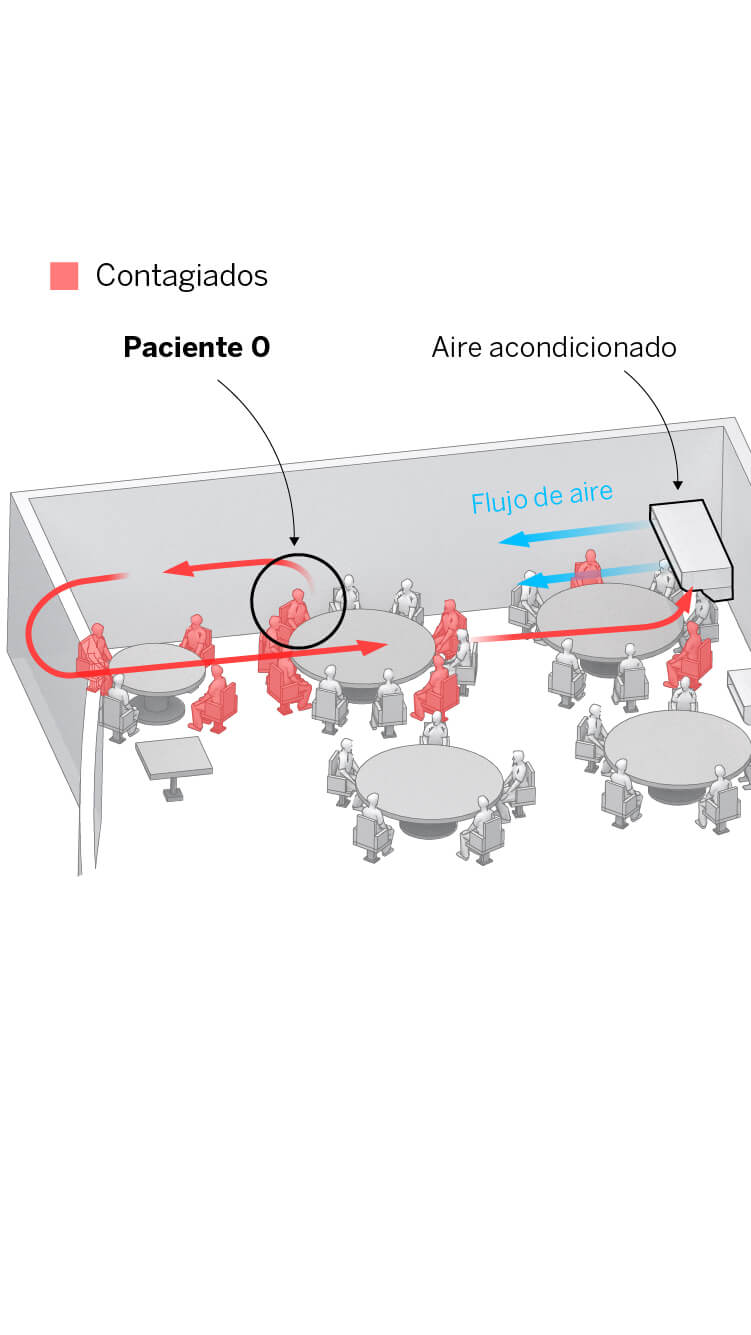
Researchers believe that the air conditioning played a crucial role. It meant the air was recirculating continuously between the three tables, concentrating the tiny, virally charged micro-droplets that Patient 0 was expelling into the atmosphere among these customers.
Cameras on the premises show that those infected had no contact in the washrooms or elsewhere that could have led to the transmission of the virus. Although close contact can play an important role in the transmission of SARS-CoV-2, transmission of the virus in small airborne droplets “in crowded, poorly ventilated rooms” is also possible, according to the scientists. Outdoor air vents in the restaurant were closed. “Our study suggests that it is vital to prevent overcrowding and provide good ventilation in buildings and public transportation to prevent the spread of SARS-CoV-2,” they add. The recommendations from the health authorities invariably insist on avoiding recirculating air, as well as holding activities outside whenever possible.
How it can be avoided
Avoid background music so people don’t have to raise their voices and expel more droplets as they speak
Open windows even if it makes people feel uncomfortably warm or cold
Avoid the recirculation of air
2 or 3 m
Reduce
the size of
indoor
gatherings
Whenever possible, hold
the event outdoors
Increase
the distance
between people
How it can be avoided
Avoid background music so people don’t have to raise their voices and expel more droplets as they speak
Open windows even if it makes people feel uncomfortably warm or cold
Avoid the recirculation of air
2 or 3 m
Reduce
the size of
indoor
gatherings
Whenever possible, hold
the event outdoors
Increase
the distance
between people
How it can be avoided
Open windows even if it makes people feel uncomfortably warm or cold
Avoid background music so people don’t have to raise their voices and expel more droplets as they speak
Avoid the recirculation of air
Always use air filters
Reduce the size
of indoor gatherings
2 or 3 m
Increase the distance between people
Whenever possible, hold
the event outdoors
How it can be avoided
Open windows even if it makes people feel uncomfortably warm or cold
Avoid background music so people don’t have to raise their voices and expel more droplets as they speak
Avoid the recirculation of air
Always use air filters
Reduce the size
of indoor gatherings
2 or 3 m
Increase the distance
between people
Whenever possible, hold
the event outdoors
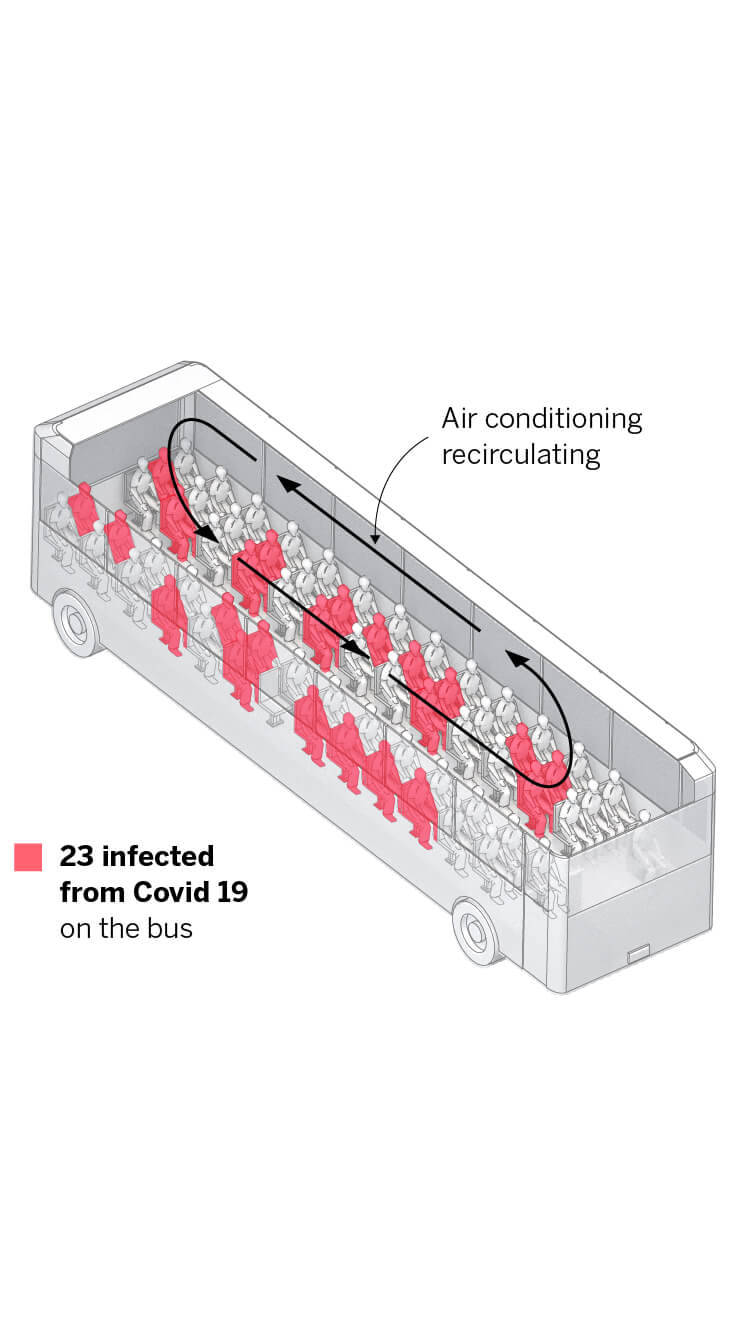
The bus
Chinese authorities and researchers from US universities are analyzing an outbreak at a Buddhist ceremony that was attended by people travelling on two buses for a total of 100 minutes – 50 minutes each way. A woman with symptoms was traveling on one of the vehicles, where the air was recirculated; 23 passengers were infected. “Patient 0 in this outbreak appears to have been a superspreader,” explains Emily Gurley, an epidemiologist at Johns Hopkins University. “As at the restaurant, transmission could be explained by aerosols and droplets traveling longer distances due to the draft from the window or the air conditioning,” she adds.
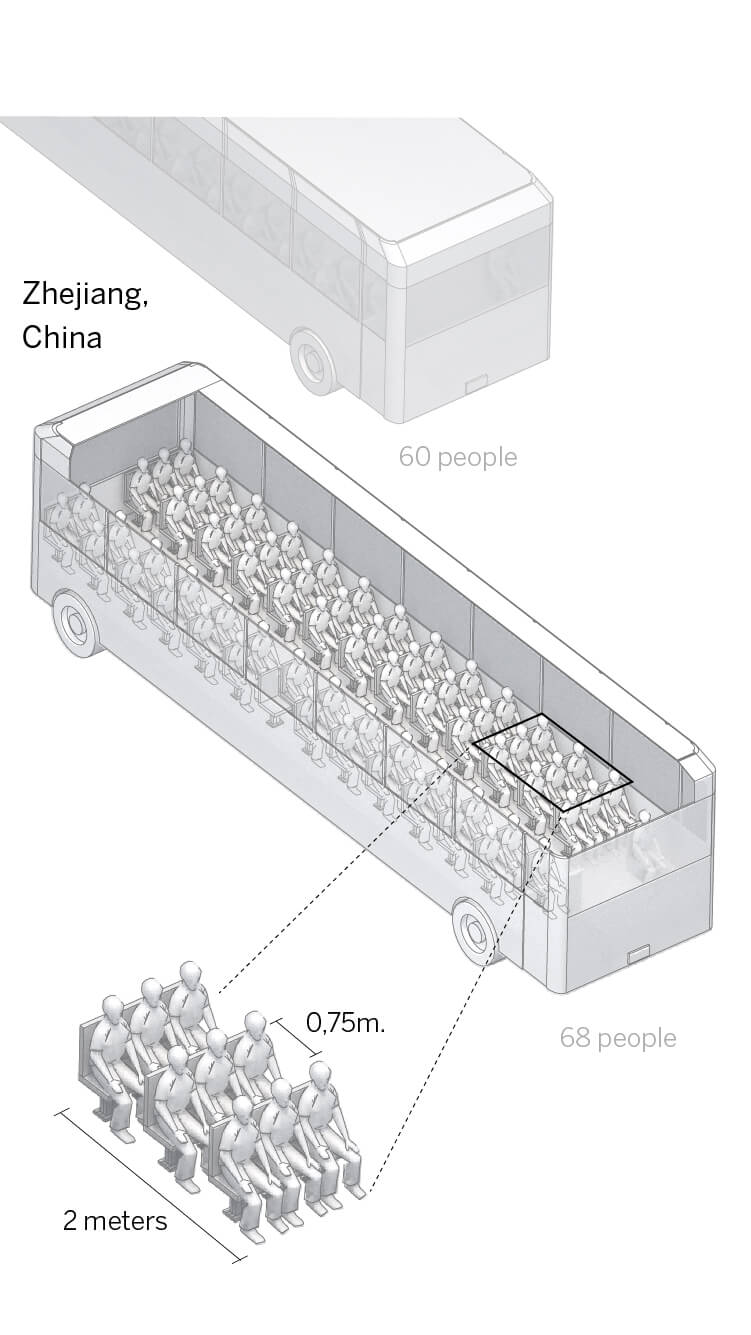
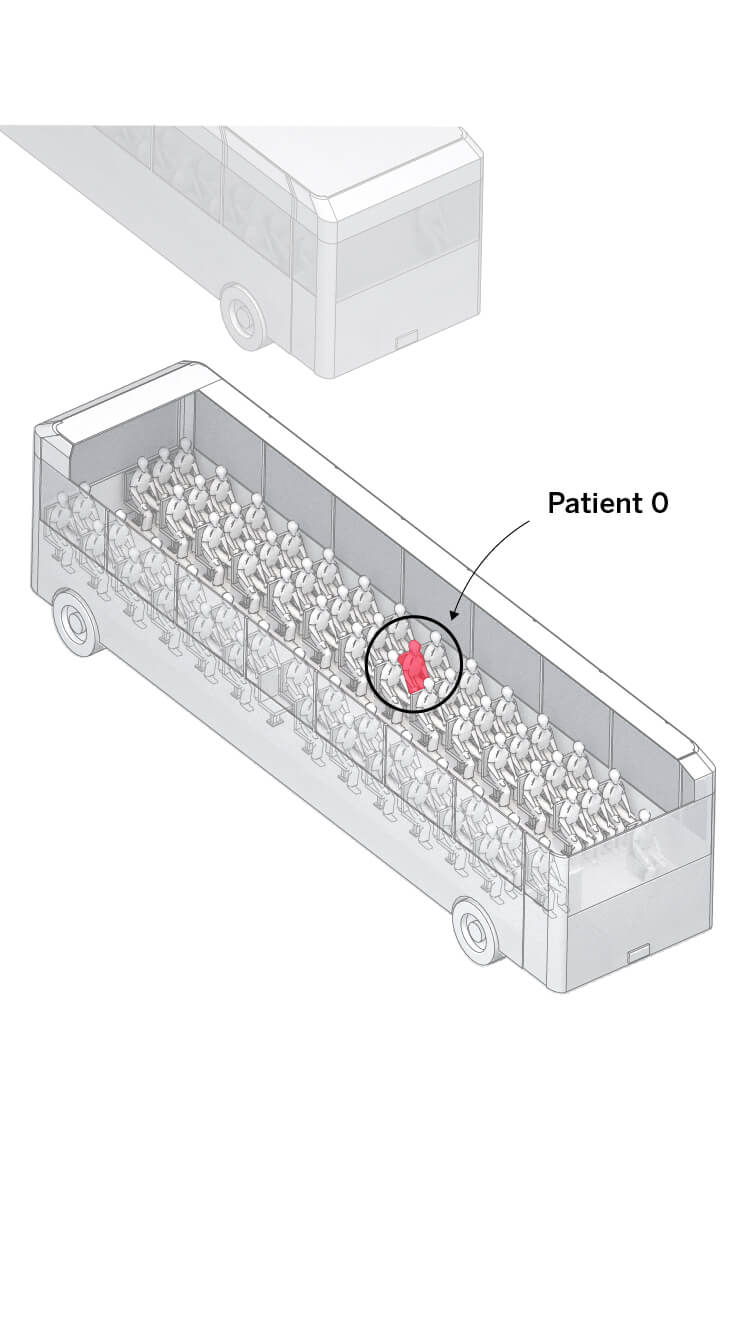


Two buses traveled to a Buddhist ceremony. The vehicles were packed, with scarcely 75 centimeters between rows.
Patient 0, a 64-year-old woman, had been in contact with people from Wuhan. She had no symptoms until the following day.
In total, 23 people got infected on the bus. No one became ill on the other bus, despite the fact they were all mixing at the ceremony.
The air conditioning was on recirculation mode. The researchers believe that this was key; the passengers became infected regardless of their distance from Patient 0.
A number of studies in Japan and elsewhere show that public transportation is not responsible for multiple infections as long as users maintain the rules of hygiene and protection, especially the use of masks that prevent infected individuals from releasing contagious droplets into the atmosphere, as happened with patient 0 on the coach. It is also suggested that specific protection measures be introduced for drivers of public transportation, as well as improving ventilation and increasing the regularity of coaches and trains in order to reduce crowding.
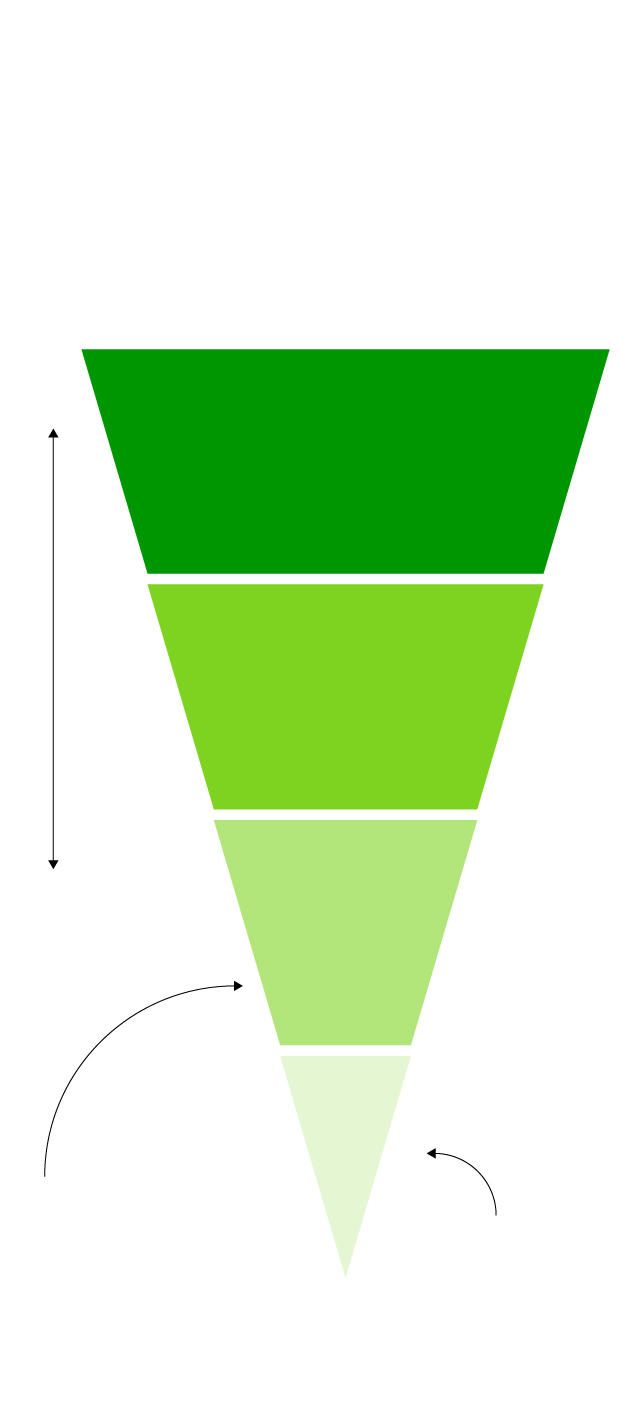
How it can be avoided
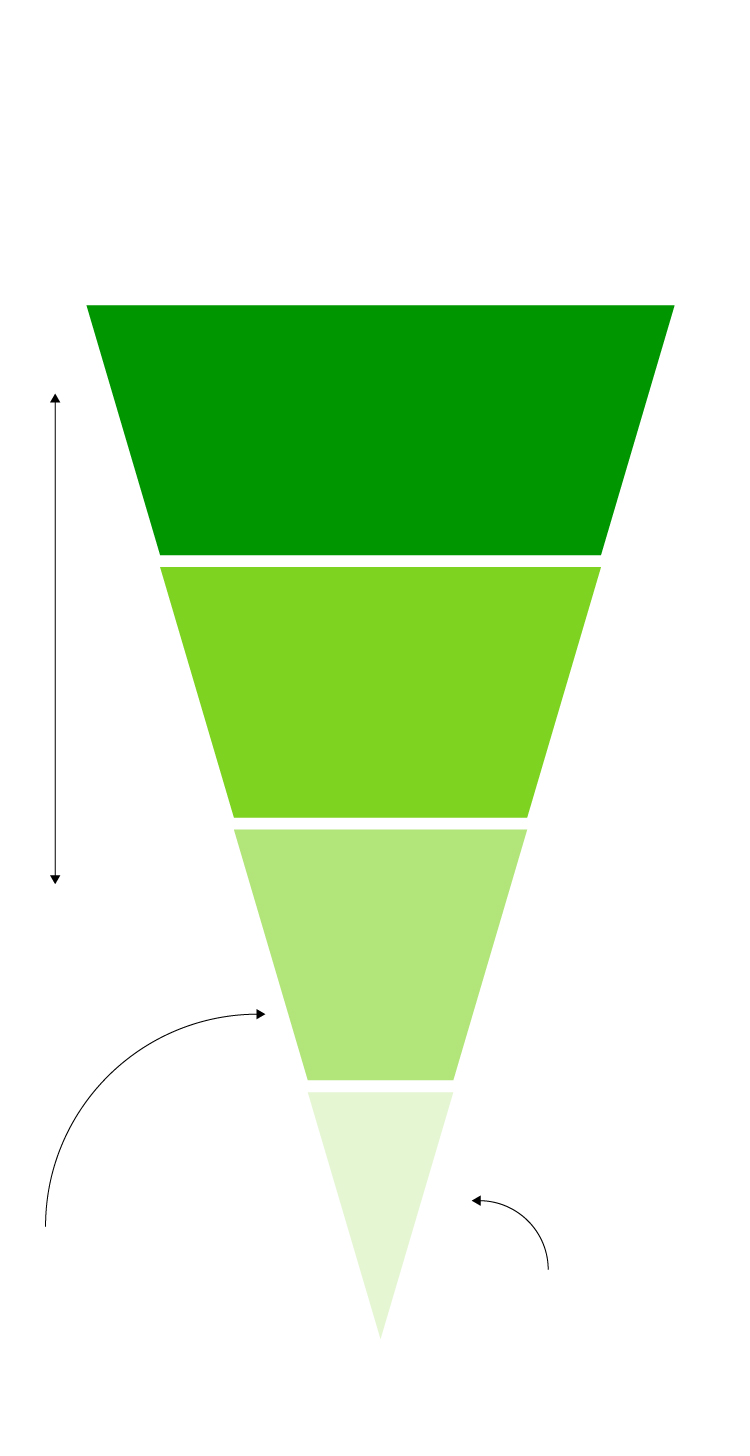
In any setting in which people are together for a prolonged period, these measures should be taken, prioritizing those that are most effective at protecting us from the risk of infection.
+
Physical distance
•Teleworking
• Reducing number
of employees in offices
Effectiveness
Engineering control
• Creating physical barriers
between people
–
Administrative
control
Protection
• Redistributing
responsibilities
to reduce contact
between people
• Mandatory use
of non-medical
masks
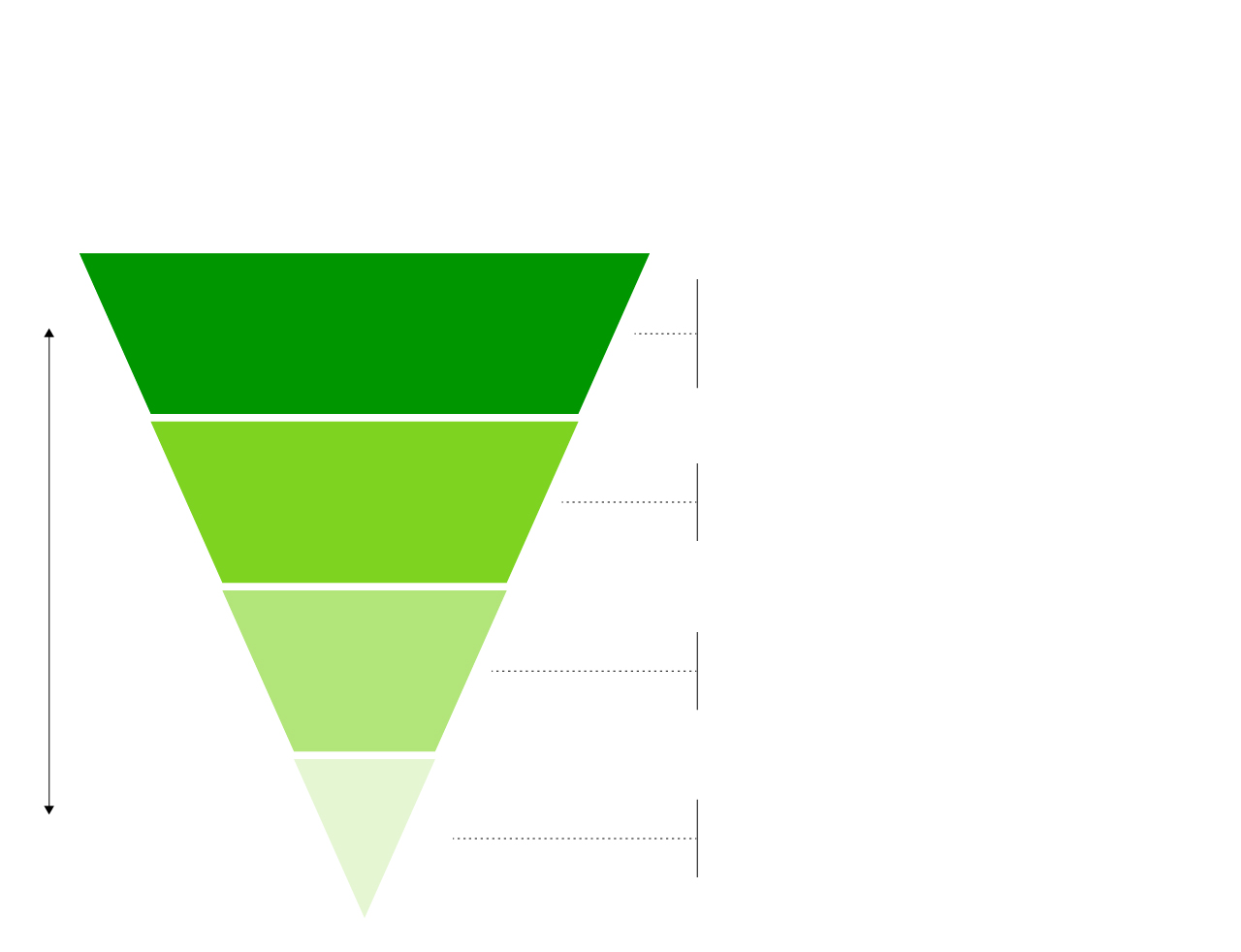
How it can be avoided
In any setting in which people are together for a prolonged period, these measures should be taken, prioritizing those that are most effective at protecting us from the risk of infection.
+
Physical distance
•Teleworking
• Reducing number
of employees in offices
Effectiveness
Engineering control
• Creating physical barriers
between people
–
Administrative
control
Protection
• Redistributing
responsibilities
to reduce contact
between people
• Mandatory use
of non-medical
masks
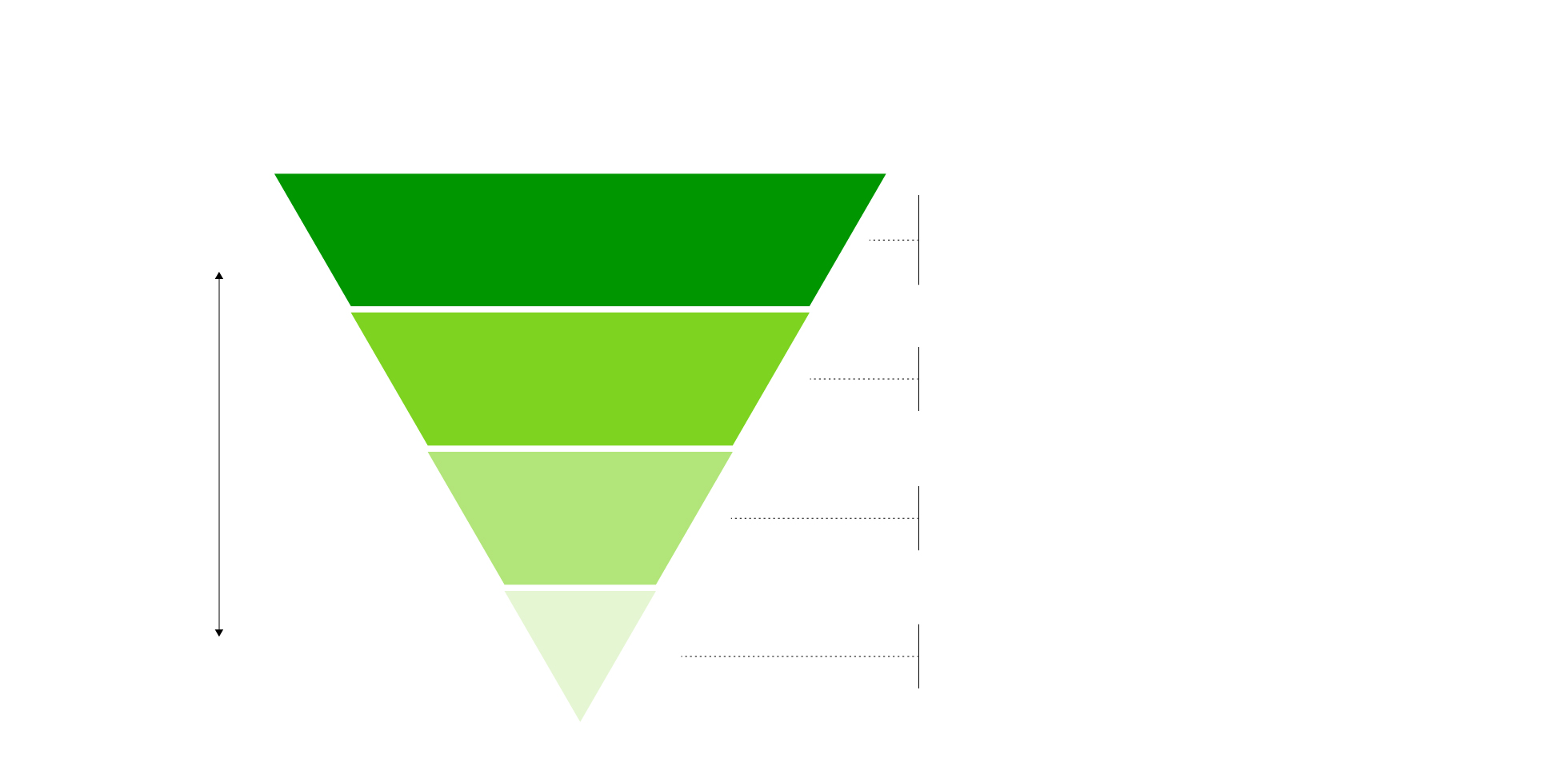
How it can be avoided
In any setting in which people are together for a prolonged period, these measures should be taken, prioritizing those that are most effective at protecting us from the risk of infection.
•Teleworking
• Reducing number
of employees in offices
+
Physical distance
Effectiveness
• Creating physical barriers
between people
Engineering control
• Redistributing responsibilities
to reduce contact between people
Administrative
control
• Mandatory use
of non-medical masks
–
Protection
How it can be avoided
In any setting in which people are together for a prolonged period, these measures should be taken, prioritizing those that are most effective at protecting us from the risk of infection.
•Teleworking
• Reducing number
of employees in offices
+
Physical distance
Effectiveness
• Creating physical barriers
between people
Engineering control
• Redistributing responsibilities
to reduce contact between people
Administrative
control
• Mandatory use
of non-medical masks
–
Protection
Effectiveness
Sources: US Centers for Disease Control and Prevention, Centers for Disease Control and Prevention in Guangzhou and Hangzhou, The Johns Hopkins Center for Health Security, the Spanish National Research Council’s Institute of Environmental Assessment and Water Studies (IDAEA-CSIC), European Centre for Disease Prevention and Control, International Laboratory for Air Quality & Health (WHO, Queensland), and the government of South Korea.
Developed by Belén Polo.